GLP-1's have been a super hot topic within the last year and I have shared my opinion about it before on social media and on the podcast, but thought I would bring together all my thoughts as I deep dive into this to get into the nitty gritty of it. Stay with me, we may get a little geeky as we dive into the different mechanisms and questions that may come up along this journey.
GLP-1 is a peptide that is largely naturally synthesized in our small intestinal mucosal L-cells and colon. It's also produced in, but at a smaller capacity, the alpha cells in our pancreas and in our brain. Since majority of it is produced within the gut, this gives a big green flag of where your health journey should focus in on. Love what GLP-1 is doing? WORK ON THE GUT. Various gut probiotics have been associated with increased GLP-1 levels, such as Akkermansia muciniphila, Bifidiobacterium animalis, etc.
Probiotics make short chain fatty acids that bind to free fatty acid receptors. This can trigger that release of GLP-1. When I go through patient's stool tests and we get to the short chain fatty acid section, I always remind them that short chain fatty acids serve the body in so many ways from metabolism to fueling your colon cells that can be protective against colon cancer. They are absolutely INCREDIBLE.
P.S. I do want to share that these drugs can be really helpful for someone who really really really needs it. But I would argue that most people that have taken it in the last couple of years probably don't.
My #1 Problem with a GLP-1
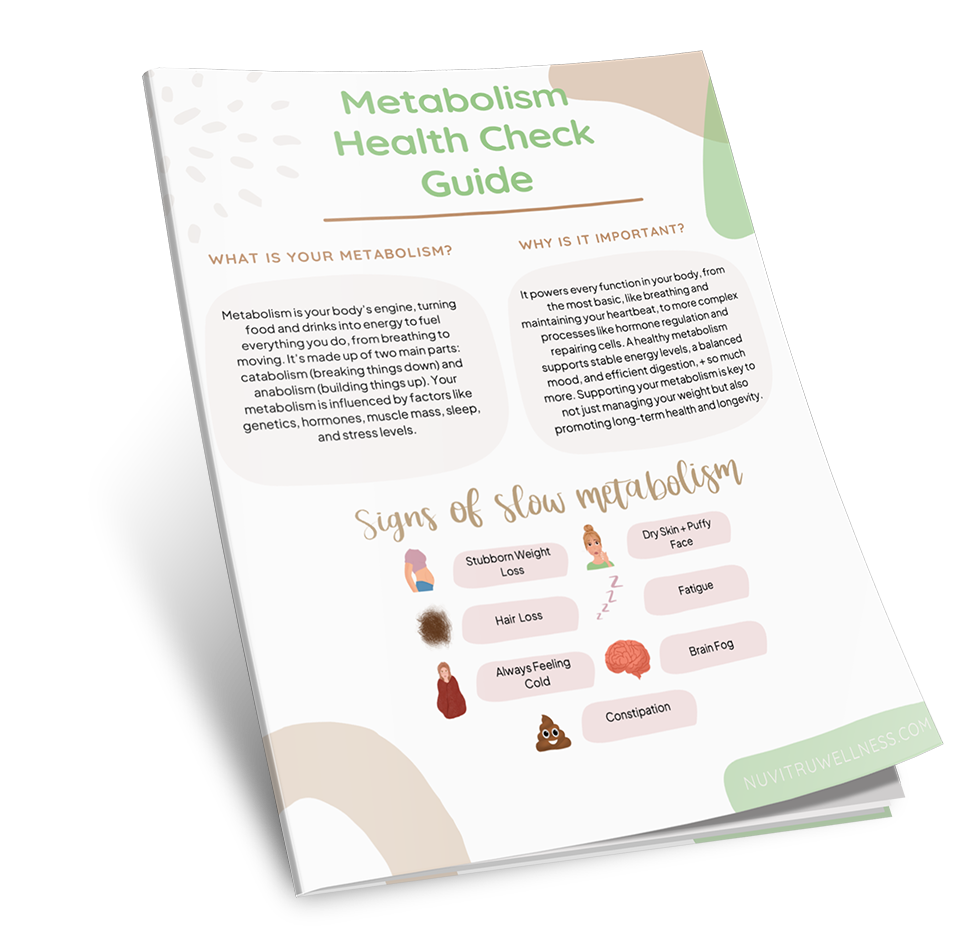
The impact that it has on appetite is my biggest pet peeve about it. The MOST common trait that I see in our patients in the last 10 years that I've been doing this is under-eating. I talk about this a lot on our socials + the downfall of under-eating is that long-term it signals to the body to hold onto weight due to starvation. The metabolism drops in response to lower calories used by the body due to this deprivation. Literal cells are slowing down in response to lower food intake. Our ghrelin hormone that makes us hungry increases (for obvious reasons) and food noise can start happening. Leptin, our satiety hormone, decreases. Cortisol, our stress hormone, rises to breakdown muscles and fat storage. With less muscle, you have less metabolic active tissue FURTHER lowering metabolism. Can't you see why people are feeling the way they are feeling?
Lowering our appetite is actually pushing our goals backwards in the long term, while there is weight loss that happens with GLP-1, there is a much bigger picture. It's the cliche saying of "you win the battle, but lose the war".
I have trouble getting people to eat more in general, now with a medication that lowers appetite it can be even MORE difficult to get enough food/fuel in their body.
*There may be conversations about microdosing a GLP-1 versus the normal doses given to most people and that these side effects wouldn't be as prominent, but I think it still comes back to our roots and understanding are we truly solving the root here?
Mechanisms Of How GLP-1's Work
Increases pancreas to release insulin to lower blood sugar
GLP-1 binds to the receptors on the beta cells of the pancreas to release insulin in response to high levels of glucose in the blood. This is why this drug is utilized for diabetes to lower glucose levels in blood because it's dangerous to have high levels of blood sugar.
BUT, a big question that me and a couple of colleague have that we have yet to find an answer from healthcare professionals, our professors, etc is the increased demand of the pancreas and the long term impacts of it. This may be a reason why pancreatitis is a rare side effect with utilizing these meds.
What to do instead:
- I wouldn't recommend doing anything to speed up insulin release per say, I would focus on getting good fiber, whole foods, balanced meals throughout the day to make sure that your blood glucose isn't spiking tremendously that requires a lot of insulin release. This means getting enough fats and proteins in our meals.
Slows down digestion
This mechanism is pretty obvious here, slowing down digestion helps someone feel less hungry (which means less fuel and increased risk of nutrient deficiencies) and can slow down the digestion of carbohydrates, which leads to a delayed response in rising blood glucose. A gut hormone, gastrin, promotes stomach emptying, but is suppressed by GLP-1s. Not only does GLP-1s slow digestion in the stomach, it slows digestion in the intestines, which can prime someone to get more constipated. This is a common side effect of these meds. This delayed digestion can also be why people feel nauseous on the medications.
As a gut health girl, I'm VERY VERY careful of what is impacting my gut because that is truly where so much of our health begins. And I don't believe that we need to be influencing our enteric nervous system to slow down.
I don't have any "what to do instead" because this is not a mechanism I would support trying to do.
Reduces appetite by GLP receptors in brain / reduces ghrelin
GLP-1 inhibits neurons that promote hunger, such as AgRP and NPY. Therefore, a person may see that reduction is desire to eating (just typing this out loud just sounds wrong, IMO). A lot of our patients may fear that their food noise is high, but I find that as we leaned into that and seeing how much they've restricted so much, it's their body pleading for nourishment that they've needed for so long. So to me, this mechanism is allowing people to eat less and restrict food intake while feeling good doing that (which is actually what is supposed to make us feel uncomfortable for good reason as food is nourishment for our body).
Speaking of appetite, GLP-1 decreases ghrelin levels, leaving you feeling full with smaller amounts of food. GLP-1 also targets the ventral tegmental area (VTA), which is a part of the brain that handles the reward system (aka our dopamine)! This med can work on dopamine signaling pathways and release.
What to do instead:
- I would work with a qualified nutrition professional that can help you lean into this. I truly deeply believe the body is INCREDIBLY smart and sometimes things our body is doing is actually it speaking to you what it needs (even if it's not something you want). As I mentioned before, I find that understanding why the body is producing hunger cues and cravings can be a game changer. Instead of fighting it, how can we listen?
- Optimizing dopamine, which can ultimately help you with food cravings and emotional eating. If there is lower dopamine levels (this can increase food cravings), prioritizing enough protein is key as it contains tyrosine that is needed for dopamine synthesis. Exercise can increase dopamine and sensitivity to dopamine to cellular receptors.
- Proper sleep quantity and quality is important because poor sleep can increase food cravings, excessive hunger (hellooo high grhelin) , and will make you want to reach for the unhealthy foods. Enough sleep is important for dopamine levels and dopamine receptors.
- Reduce your stress as this is a big trigger for appetite changes
Increases muscle glucose uptake
GLP-1s can make the glucose transporters more sensitive to insulin. These glucose transporters can be found on the muscle, one specifically is GLUT4. Having poor glucose muscle uptake can contribute to type 2 diabetes.
What to do instead
- Building muscle!!! Strength training that involves growing muscle increases GLUT4 protein production and translocation (aka bringing GLUT4 from inside the cell to the membrane of the cell). This helps increase insulin sensitivity and glucose uptake into the cell.
- Love this mechanism of GLP-1? Go back to where GLP-1 is made (aka gut health) and make sure that your body is naturally producing this optimally.
Reduces glucagon secretion
Glucagon is released by the alpha cells in the pancreas and it causes the liver to released stored glucose, which ultimately raises blood sugar! This is an essential hormone that we use during fasting to keep your blood glucose levels stable. So, the GLP-1 drug inhibits glucagon release by binding to those alpha cell receptors, which stops any increased blood glucose levels (which can actually lead to hypoglycemia at times).
I wouldn't recommend wanting to reduce glucagon secretion per say, but aim for balancing any dysregulated glucagon secretion. This often stems from hyperglycemia, which we should assess diet and lifestyle as that is usually the biggest trigger for that and mitochondrial/cellular issues. One of the reasons cellular function can be impacted is problems with intracellular sodium accumulation. A way to improve sodium balance inside the cell is working with the sodium-potassium pump. One way to increase activity of this pump as increasing magnesium intake. A magnesium deficiency doesn't change the number of pumps a cell has, but it can impact the activity.
Glucagon secretion can become dysregulated by having a fatty liver. Fatty liver can make the liver resistant to glucagon, so now, we want to peel back the layers of what is causing fatty liver. We've seen so much improvement with this in our patients who work on their diet and lifestyle.
Reduces inflammation
Another mechanism that GLP-1s can work is by reducing the production of inflammatory cytokines, such as IL-6. Getting real geeky, it downregulates the NF-xB pathway, which is a major pathway in regulating inflammation levels in the body.
What to do instead:
- Understand WHAT is causing inflammation in the first place. This is the true root cause work of inflammation. A lot of this lies within diet, emotional/mental health/stress, and lifestyle.
- There are other natural herbs that can reduce inflammatory cytokines, such as boswellia. Boswellia is shown in studies to down-regulate the NF-xB pathway too! Even though these are still natural band-aids, they can be helpful while working through the root cause.
- Omega-3's can be helpful in inflammation regulation and can also improve insulin sensitivity that allows your body to use glucose properly.
With all of this information, the goal is to show you that it still boils down to the basics. While GLP-1 may give you a head start or upper-edge, I'm still a proponent of using drugs as sparingly as possible.
As you go through this mechanisms, you may still think "but it all comes down to dose" as microdosing becomes a bit more popular, but I still want you to ask yourself if I take this, "am I actually solving the root cause?" Are we truly understanding why you may be insulin resistant or you have blood sugar dysregulation in the first place? Are we truly understanding why you struggle with food noise? Are we truly understanding why our metabolism may be lower in the first place?
Are we really going to make those root cause hard decisions that are impacting your life that may be a reason why blood sugar regulation or stubborn weight loss is happening in the first place?
Because I've seen it before, people get results, they get comfy, ease up on the search of the root cause because they already have their results, so they don't put as much emphasis on changing the diet or lifestyle habits. They can keep enjoying certain habits that aren't serving them because their external or internal goals are met (I lost x amount of weight or my fasting glucose is under 100 now).
From some of the stats I've seen, following the withdrawal of the medication people regained 2/3rd's of the weight loss and cardiometabolic variables went back to baseline in the long-run.
If you ARE on semaglutide, there should a plan to get off of it and if your practitioner states that there isn't a way for you to get off, this is a red flag that you actually didn't do root cause work.
Connect With Us
Resources Mentioned
- Work with our team if you are looking to get our exclusive January bundle that will give you the data that you need!


-1.png)